Understanding Polyarthritis: Causes, Symptoms, and Treatment Approaches
Polyarthritis is a common musculoskeletal disorder that affects multiple joints in the body, causing pain, stiffness, and reduced mobility. Understanding its causes, symptoms, and treatment options can help improve quality of life and prevent severe complications. Explore more in the article below!
What Is Polyarthritis?
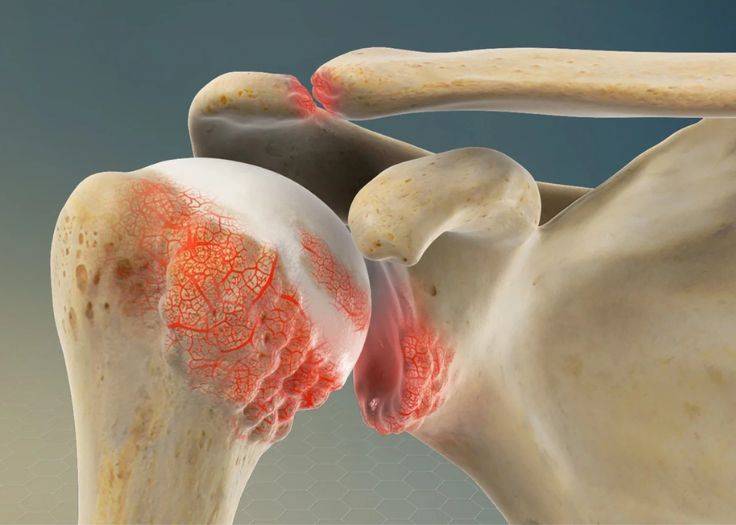
Polyarthritis refers to the gradual degeneration of the protective cartilage covering the ends of bones in multiple joints. This cartilage serves as a cushion, reducing friction and ensuring smooth joint movement. When it deteriorates, it becomes thinner, loses elasticity, and becomes more vulnerable to damage.
This degenerative process commonly affects frequently used joints such as the shoulders, neck, knees, ankles, and wrists. When osteoarthritis develops in two or more joints, it is classified as polyarthritis. Over time, the disease progresses and cannot be completely reversed.
As cartilage breaks down, the bones may rub directly against each other, causing pain, swelling, and stiffness. In more advanced cases, bone spurs may form, altering the joint structure. Severe cartilage loss can also lead to bone misalignment, resulting in persistent discomfort and restricted movement.
Polyarthritis osteoarthritis occurs when the cartilage tissue is damaged.
Symptoms of Polyarthritis
Arthralgia: The primary symptom of polyarthritis presenting as pain that ranges from mild discomfort to severe, debilitating pain. Symptoms often worsen with movement and improve with rest, with pain sometimes radiating to surrounding structures.
Joint Stiffness: Affected joints can restrict movement and cause discomfort., especially in the morning or after prolonged inactivity.
Swelling and Inflammation: Damaged joints may exhibit swelling, warmth, and redness due to inflammation.
Crepitus and Joint Locking: Some individuals may experience a cracking or grinding sensation during joint movement. In some cases, the joint may feel locked or restricted, limiting mobility and causing discomfort.
Common Complications of Polyarthritis
Joint Deformity: Over time, joint degeneration may cause structural changes, such as joint swelling, bone spur formation, and articular surface irregularities, which may result in joint misalignment.
Limited Mobility: The loss of cartilage and joint stiffness can reduce flexibility, restricting the range of motion. Activities such as walking, climbing stairs, and performing daily movements become increasingly challenging.
Deterioration in Quality of Life: Chronic pain and mobility impairment can significantly impact daily activities, work productivity, and overall well-being. Persistent discomfort may also contribute to psychological distress, including anxiety and depression.
Disability: In severe cases, polyarthritis can lead to severe joint destruction, causing permanent disability and loss of independence in daily activities.

Causes of Polyarticular
Polyarticular osteoarthritis develops due to various factors, including:
Trauma and Repetitive Joint Injuries: Previous joint injuries or repetitive stress on the joints can accelerate degeneration. Athletes and individuals engaged in physically demanding activities have an increased risk due to chronic joint overload.
Obesity and Excess Body Weight: Excess body weight places significant stress on weight-bearing joints, such as the knees and hips, leading to increased cartilage wear and a higher risk of polyarthritis.
Pre-existing Joint Conditions: Conditions such as rheumatoid arthritis, gout, and chronic synovitis predispose individuals to secondary osteoarthritis due to persistent inflammation and structural joint damage.
Occupational and Lifestyle Factors: Prolonged engagement in occupations requiring heavy lifting, kneeling, or repetitive joint movements can accelerate degenerative joint changes over time.
Aging and Cartilage Degeneration: Advancing age is a primary risk factor, with individuals over 50 experiencing increased cartilage wear, reduced synovial fluid production, and progressive joint deterioration.
Gender Differences: Postmenopausal women have a higher prevalence of polyarticular osteoarthritis due to hormonal changes affecting cartilage metabolism. In younger individuals, men are more prone to osteoarthritis linked to occupational hazards and high-impact activities.
Genetic Susceptibility: A family history of osteoarthritis suggests a genetic predisposition, influencing cartilage integrity, joint structure, and inflammatory responses that contribute to disease onset.

Effective Treatment Options for Polyarticular Osteoarthritis
Several treatment approaches are commonly used to manage polyarticular osteoarthritis, including:
Pain Relief and Anti-inflammatory Medications
Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and naproxen help reduce pain and inflammation in affected joints. Acetaminophen (paracetamol) may also be used for pain management. In some cases, corticosteroid injections are administered directly into the joint to provide localized pain relief and reduce inflammation.
Physical Therapy
A structured physical therapy program, including massage, electrical stimulation, ultrasound therapy, and functional exercises, can improve joint flexibility, reduce pain, and enhance mobility.
Joint Support Devices
Assistive devices such as canes, braces, or crutches may be recommended to alleviate joint stress during movement, reducing pain and preventing further damage.
Surgical Intervention
For severe cases that do not respond to conservative treatments, surgical options may be considered. Procedures such as osteophyte (bone spur) removal or total joint replacement can help restore joint function and relieve pain.
Lifestyle Modifications
Maintaining a healthy lifestyle is crucial in managing osteoarthritis. Weight control helps reduce stress on weight-bearing joints, while regular low-impact exercise strengthens muscles and improves joint flexibility. Avoiding activities that place excessive strain on the joints can also help slow disease progression.
Platelet-Rich Plasma (PRP) Therapy
PRP therapy is an emerging regenerative medicine technique for osteoarthritis management. It involves using the patient’s own blood, which is processed to concentrate platelets and growth factors that promote tissue regeneration, reduce inflammation, and enhance healing.
PRP contains high levels of biologically active proteins, including platelet-derived growth factor (PDGF), transforming growth factor-beta (TGF-β), and vascular endothelial growth factor (VEGF), which support cell proliferation, new blood vessel formation, and inflammation reduction. When injected into damaged joints, PRP accelerates the body’s natural healing process.
Advantages of PRP therapy include:
Minimally invasive and quick procedure
Low risk of immune reaction as it uses the patient’s own blood
Cost-effective compared to surgical alternatives
Understanding polyarticular allows individuals to take preventive and timely treatment measures. Regular medical check-ups, a balanced diet, appropriate exercise, and adherence to medical recommendations play a crucial role in protecting joint health and improving overall quality of life.










